Despite ongoing left lies, per usual.
Medicaid
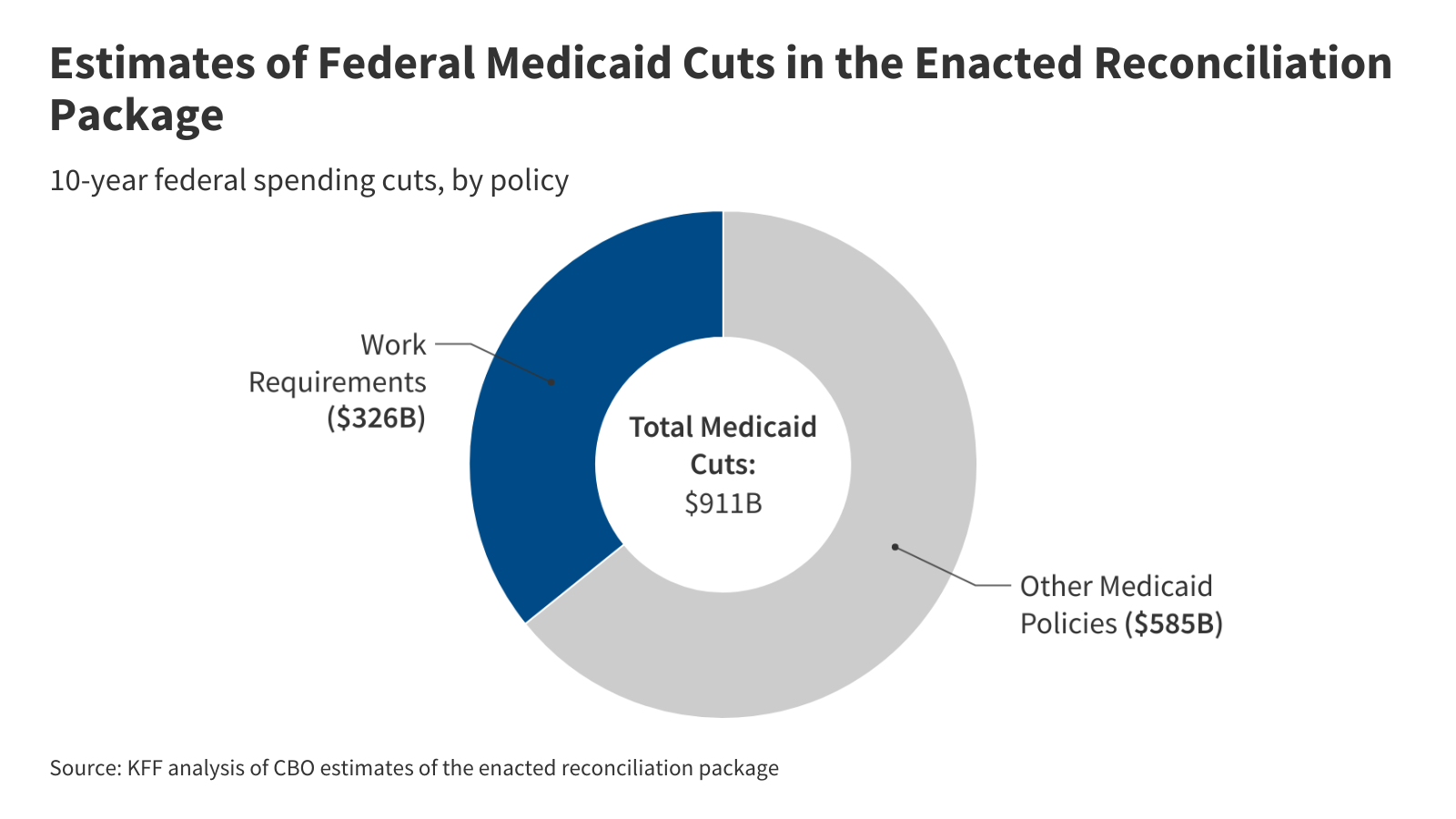
Work Requirements
- Overview: Requires able-bodied adults aged 19-64 to work (or perform other qualifying activities) for at least 80 hours a month. There are mandatory exemptions for certain individuals (e.g., pregnant women, those with serious medical conditions, tribal members, parents/caregivers of a dependent child 13 years and under or with a disability). States may issue optional hardship waivers for specific individuals facing short-term hardship (e.g., inpatient care, related outpatient care, natural disasters, high unemployment rate within their county).
- Verification: States will be required to conduct a “look-back” to determine if an individual meets requirement within the three months prior to applying. States would be required to verify an individual's compliance with work requirements within one or more months of enrollment and one or more months before redetermination.
- Implementation Dates:
- June 1, 2026: HHS to release interim final rule with implementation requirements.
- Dec. 31, 2026 (or earlier at state option): States must implement work requirements. However, the final bill allows the Secretary to exempt states from compliance with new requirements until Dec. 31, 2028, if they demonstrate a good faith effort toward compliance.
- Funding: Provides $200M for HHS implementation funding and $200M for states in FY2026 (an increase from $50M and $100M, respectively, from the initial House version).
Expansion
- Expansion FMAP for Emergency Medicaid: Effective Oct. 1, 2026, limits federal matching payments for Emergency Medicaid to the state’s regular FMAP for individuals who would otherwise be eligible for coverage through Medicaid expansion if not for their immigration status.
- Sunsetting increased FMAP incentive: Effective Jan. 1, 2026, states that newly adopt Medicaid expansion will no longer have provisions for the temporary incentive. In addition to the federal government providing 90% federal financing for the expansion population under a state’s Medicaid expansion, the American Rescue Plan Act provided states that expand Medicaid after March 2021 a temporary boost in FMAP — a two-year, five-percentage-point increase in FMAP for all non-expansion population.
- Modifying cost sharing requirements for certain expansion individuals under Medicaid: Effective Oct. 1, 2028, states are required to impose cost sharing of up to $35 per service on expansion adults with incomes 100-138% FPL. Exempts primary care, mental health, and substance use disorder services, along with services provided by federally qualified health centers (FQHCs), behavioral health clinics, and rural health clinics. Maintains the previous law that out-of-pocket costs cannot exceed 5% of family income. Provides $15M in implementation funding for 2026.
- The final legislation adds exemptions to cost-sharing services provided by FQHCs, behavioral health clinicals, and rural health clinics.